Being told a tooth needs a root canal can feel intimidating, but modern root canal therapy is a predictable, routine treatment designed to relieve pain and preserve your natural tooth. Advances in instruments, imaging, and techniques mean the experience today is much more comfortable than many people expect, and the end result helps protect both your oral health and your smile.
At the office of Wells Dentistry, we combine careful diagnosis with gentle treatment to help patients avoid unnecessary extractions and keep teeth functioning for years to come. Our approach focuses on clear explanations, precise care, and helping you understand what to expect at every step.
When a tooth’s inner tissues become inflamed or infected, removing that tissue and sealing the tooth can prevent the problem from spreading and maintain the structural integrity of your bite. Keeping a natural tooth helps preserve surrounding teeth, supports jawbone health, and avoids the long-term challenges that can come with replacing teeth.
Root canal therapy has a strong track record of success when performed in a timely and thorough manner. With appropriate restoration after treatment, many teeth with root canal therapy continue to serve their function for decades. Opting to save a tooth rather than remove it often means fewer future procedures and a more natural outcome.
Decisions about whether to pursue root canal treatment are always individualized. We evaluate the overall condition of the tooth, the amount of remaining structure, and the state of the supporting bone to determine the most predictable path forward for long-term health.

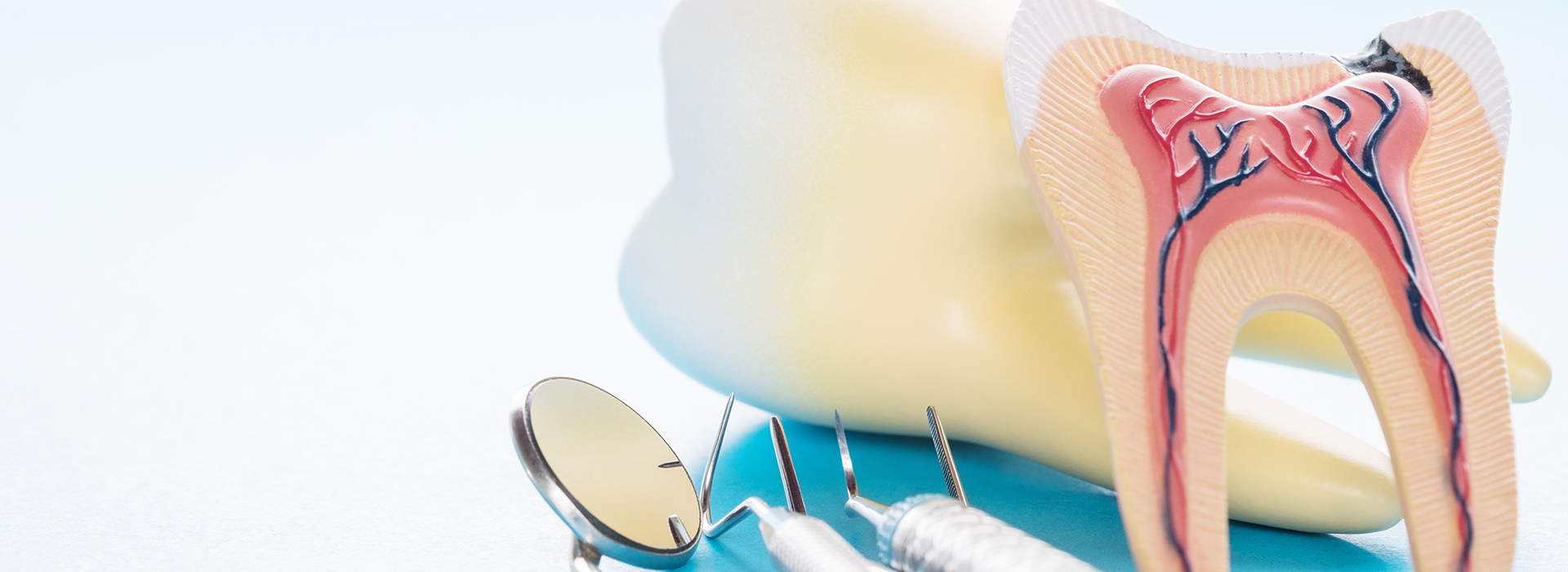
Teeth aren’t just hard surfaces — they contain a central pulp chamber made up of nerves, connective tissue, and blood vessels. When this tissue becomes irritated by deep decay, trauma, or repeated dental work, it can lead to symptoms that warrant evaluation for root canal therapy.
Symptoms can range from dull, persistent discomfort to sharp pain with biting, or lingering sensitivity to hot and cold. Not every painful tooth needs a root canal, but these signs are your body’s warning that a closer look is necessary to prevent progression.
Some affected teeth show visible clues like discoloration, swelling, or increased mobility. Others may be asymptomatic but reveal problems on X-rays. Early assessment improves the chances of a straightforward, successful outcome.
Below are common indicators that a tooth may require root canal treatment:
Persistent pain, especially pain that wakes you from sleep or comes in waves, often signals deep decay or nerve involvement. While many dental conditions can cause discomfort, this pattern is one of the more frequent reasons a clinician will recommend root canal therapy.
Teeth that react strongly or lingeringly to hot or cold can indicate that the pulp is inflamed. If sensitivity persists long after the stimulus is removed, it’s an important symptom to investigate.
Discomfort with pressure or light contact may suggest the infection or inflammation is affecting the supporting tissues and nerve endings. Addressing this early can help prevent more extensive problems.
A tooth that becomes discolored after trauma or over time can indicate internal changes to the pulp. While not every darkened tooth needs a root canal, it’s a sign that merits diagnostic attention.
If an injury exposes or damages the inner tissues, the pulp can become compromised. Even seemingly minor chips can lead to deeper problems if bacteria reach the pulp chamber.
Localized gum swelling, a tender lump, or an area that drains are signs that an infection may be present. These symptoms require prompt evaluation and treatment to prevent spread.
If supporting bone is affected by infection, the tooth may feel loose. Root canal therapy can stop the infectious process and allow healing of the surrounding tissues in many cases.

When symptoms like those described appear, scheduling a timely exam helps limit complications. Some teeth show few, if any, early symptoms yet already have changes at the root tip visible on X-rays. That’s why regular dental exams and radiographs are key to catching problems before they worsen.
Delaying care increases the likelihood that infection will extend beyond the tooth and into adjacent bone or soft tissues, potentially complicating treatment and recovery. Treating an affected tooth promptly improves predictability and typically reduces discomfort for the patient.
Your dentist will explain the findings, the reasons for recommending root canal therapy (if indicated), and the anticipated steps for restoring the tooth afterward. This collaborative approach helps you make a confident, informed decision about care.
Root canal treatment removes the diseased pulp, cleans and shapes the root canals, and seals them to prevent recontamination. The process is performed with local anesthesia to keep you comfortable, and many techniques today allow for precise cleaning using modern files and irrigation systems.
Some treatments can be completed in a single visit, while others require two or more appointments depending on the tooth’s anatomy, the presence of infection, and whether additional procedures (such as placement of a post or core) are needed. Your clinician will outline the expected timeline based on the specific case.
Following the root canal, the tooth typically needs a permanent restoration — often a crown — to restore strength and function. A well-sealed restoration protects the treated tooth from fracture and new leakage, contributing to a favorable long-term prognosis.

After treatment, it’s normal to experience some tenderness around the treated tooth as surrounding tissues recover. This discomfort usually lessens over a few days. Over-the-counter anti-inflammatory medications are often recommended to manage discomfort; if a prescription is needed, your clinician will provide one.
Protecting the treated tooth until a permanent restoration is placed is important. Temporary fillings or restorations are not as strong as final crowns and can be vulnerable to fracture or leakage. Avoiding hard foods on that side until the tooth is fully restored helps prevent complications.
Continue routine brushing and flossing and attend follow-up visits so your dentist can confirm healing. With appropriate restoration and good oral hygiene, a tooth that has undergone root canal therapy can remain functional for many years — often for a lifetime.
At the office of Wells Dentistry, our team is committed to delivering careful, evidence-based endodontic care and to answering your questions along the way. If you have signs of an infected or painful tooth, or if you’d like to learn whether root canal therapy is the right option for you, please contact us for more information.

Root canal therapy treats the diseased or injured dental pulp, the soft tissue inside a tooth that contains nerves and blood vessels. The procedure removes inflamed or infected pulp to stop pain and prevent the spread of infection to surrounding bone and tissues. It is a targeted way to preserve the natural tooth rather than resorting to extraction.
After cleaning and shaping the canal system, the space is sealed to reduce the risk of reinfection and to restore function. Preserving the natural tooth helps maintain proper chewing, supports adjacent teeth, and protects jawbone structure. Decisions about treatment are individualized based on the tooth’s condition and overall oral health.
Common symptoms that prompt evaluation for a root canal include persistent toothache, prolonged sensitivity to hot or cold, and pain when biting or with pressure. Some patients notice swelling, a pimple-like bump on the gum, or a darkening of the affected tooth. Other times the tooth becomes loose or shows signs of infection on the gum tissue. Not every painful or sensitive tooth requires a root canal, but these signs indicate the need for prompt assessment.
Your dentist will use clinical tests and diagnostic imaging such as X-rays to determine whether the pulp is compromised and to assess the extent of infection. In some cases a tooth may be asymptomatic yet show changes at the root tip on radiographs. Early diagnosis improves treatment options and outcomes.
A modern root canal begins with local anesthesia to make the tooth numb and comfortable for treatment. The clinician creates a small access opening to reach the pulp chamber, then removes diseased tissue and cleans and shapes the root canals using files and irrigating solutions. Contemporary techniques often employ rotary instruments, magnification, and enhanced irrigation to improve cleanliness. The canals are then filled and sealed to prevent recontamination.
Some root canals are completed in a single visit while others require two or more appointments depending on anatomy and infection control needs. A temporary restoration protects the tooth between visits until a permanent restoration is placed. Patients receive clear aftercare instructions and the clinician will explain the expected timeline for final restoration.
Local anesthesia makes modern root canal treatment comfortable for the vast majority of patients, and many people report little to no pain during the procedure. Preoperative pain is commonly caused by infection or inflammation of the pulp rather than the treatment itself. Addressing the problem often brings significant relief once the infection is removed.
After the appointment some tenderness or mild soreness around the treated tooth and surrounding tissues is normal as healing begins. Over-the-counter anti-inflammatory medications usually control post-procedure discomfort, and the dentist can advise if additional medication is needed. If severe or worsening pain, swelling, or changes in sensation occur, contact your dental office promptly for evaluation.
Care after a root canal focuses on protecting the treated tooth and supporting healing of the surrounding tissues. Avoid chewing on the treated side until a permanent restoration is placed to prevent fracture of a temporary filling. Continue gentle brushing and flossing, paying attention to the area while it heals to keep bacterial levels low. Maintain any medications or instructions provided by your dentist to support recovery.
Attend follow-up visits so the clinician can confirm healing with a clinical exam and, if needed, radiographs. Report any persistent pain, swelling, or new symptoms promptly so they can be evaluated and managed. Long-term success depends on a well-sealed final restoration and good oral hygiene.
Many teeth that undergo root canal therapy, especially molars and premolars, require a crown or other full coverage restoration to restore strength and protect against fracture. Front teeth with simpler anatomy sometimes can be restored with a bonded filling depending on the remaining tooth structure. The purpose of a permanent restoration is to seal the tooth against bacterial reentry and to restore normal function. Your dentist will recommend the most appropriate restorative option based on the tooth’s location, remaining structure, and functional demands.
Placement of the final restoration is a critical step in the long-term success of the treated tooth and should not be delayed once healing is established. Well-fitting crowns and restorations help distribute biting forces and reduce the risk of future problems. Regular checkups will allow the dentist to monitor the restoration and the treated tooth over time.
A tooth treated with root canal therapy can last many years and often remains functional for the lifetime of the patient when properly restored and cared for. Longevity depends on factors such as the quality of the root canal filling, the type of final restoration, the patient’s oral hygiene, and the amount of remaining tooth structure. Teeth subjected to heavy biting forces or with extensive structural loss have a higher risk of fracture over time.
Occasionally a treated tooth may require retreatment, endodontic surgery, or extraction if persistent infection or structural failure occurs. Regular dental examinations and radiographs help detect and address problems early, improving the long-term prognosis. At Wells Dentistry, the team emphasizes careful restoration and monitoring to maximize treatment outcomes.
General dentists provide many root canal treatments, but a referral to an endodontist is common for teeth with complex root anatomy, previous failed root canal therapy, or when surgical intervention may be necessary. Endodontic specialists have additional training and tools such as operating microscopes and advanced imaging to navigate difficult canal systems. They frequently manage teeth with curved or calcified canals, re-treat failed cases, and perform apical surgery when nonsurgical retreatment is not feasible. Your general dentist will discuss the benefits of specialist care when it is the most predictable option.
Collaboration between the general dentist and endodontist ensures the tooth receives appropriate restorative work after endodontic treatment. In many cases the general dentist will place the final crown or restoration once the root canal is complete. This team approach focuses on preserving the tooth and restoring full function.
Root canal treatment is generally safe, but like any procedure it carries potential complications such as incomplete cleaning of a complex canal, instrument separation, or accidental perforation of the root. Persistent or recurrent infection can occur if bacteria remain or re-enter the canal system, and additional treatment such as retreatment or surgery may be necessary. There is also a small risk of postoperative swelling or sensitivity as the tissues heal. Most complications are manageable when identified and treated promptly.
Good communication with your dental team and adherence to follow-up appointments reduce the likelihood that problems will go unrecognized. If signs such as increasing pain, swelling, persistent drainage, or unusual symptoms develop after treatment, return to the dental office for evaluation. Early intervention leads to better outcomes than delayed care.
You can lower your risk of needing root canal therapy by maintaining excellent daily oral hygiene, including thorough brushing, flossing, and using fluoride products as recommended. Address cavities, cracked teeth, and failing restorations promptly so that minor problems do not advance to pulp involvement. Wearing a protective mouthguard during sports and avoiding hard or injurious habits also helps prevent traumatic damage that can lead to pulp injury. Regular dental checkups and radiographs allow your dentist to catch early signs of decay or internal changes before they require root canal treatment.
Lifestyle factors such as smoking and uncontrolled systemic conditions can impair healing and increase risk of dental problems, so managing overall health supports oral health. If you have specific concerns about tooth pain or a high risk for dental decay, discuss targeted prevention strategies with your dental team. Early action and consistent care are the most effective ways to preserve natural teeth and avoid more invasive treatment.

It's time for your check-up!
Scheduling your next visit or getting answers about our comprehensive dental services is simple when you contact Wells Dentistry. Our friendly administrative team is prepared to help you find the perfect appointment time, provide clarity on your treatment plan options, and efficiently manage any billing or insurance questions. We are ready to assist you by phone or via our quick online form. Contact us today and let us partner with you to maintain a healthy, beautiful smile for years to come.